Arthritis is a common, yet painful disease that causes joint inflammation in the body. Though it can affect any joint, many people have arthritis of the foot and ankle, where tiny joints are responsible for supporting the body’s weight and absorbing shock. Arthritis causes the joints to swell and become inflamed, leading to severe pain. Often, a person with advanced stages of arthritis will experience sensations of bone rubbing on bone as the cartilage deteriorates and results in bone spurs.
Did you know…
there are more than 100 types of arthritis? Many of them can affect the joints of the foot and ankle, causing pain and stiffness. According to the Centers for Disease Control, more than 52 million adults – 1 in 5 – have been diagnosed with some form of arthritis in the U.S. Of them, many suffer from debilitating foot and ankle pain that makes even the simplest everyday tasks like walking or exercising much more complicated.
Frequently Asked Questions
What causes foot and ankle arthritis?
A person can develop foot and ankle arthritis as a result of many different causes or ‘triggers’. For example, osteoarthritis is a degenerative disease in which the cartilage surrounding a joint slowly wears down. Injuries can also cause the disease to develop, resulting in posttraumatic arthritis. Another type of arthritis – rheumatoid arthritis – is an autoimmune condition that causes the body’s immune system to attack the tissues of the joint. Though the disease is not believed to run in families, certain people – particularly those who are obese – are at a heightened risk of developing it.
What are the symptoms of foot and ankle arthritis?
A person with foot and ankle arthritis will have varying degrees of symptoms depending on how advanced the disease is. However, this condition typically causes stiffness and pain when walking or standing, as well as tenderness when pressure is applied to the joints. The joint may also swell or become warm to the touch, and in many cases it is worse in the mornings or when participating in vigorous activity.
How will a podiatrist treat foot and ankle arthritis?
There are many different ways of treating foot and ankle arthritis. Though there is no cure, the focus is often on symptom management and slowing the progression of the disease. At our office, we emphasize a non-surgical and minimally invasive approach, which may include lifestyle modifications, orthotics and the use of advanced and alternative therapies. For more information about foot and ankle arthritis treatment, contact our office to schedule a consultation.

 Featured Services
Featured Services

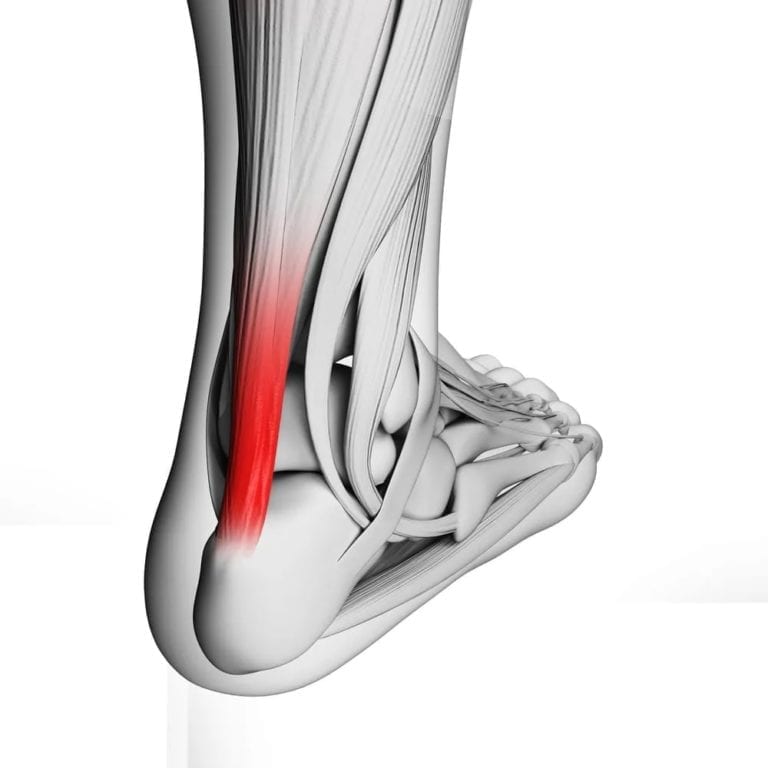
 condition characterized by the degeneration and inflammation of the Achilles tendon. The Achilles tendon is a strong band of tissue that connects the calf muscles to the heel bone. Often, a painful spur is present on the back of the heel.
condition characterized by the degeneration and inflammation of the Achilles tendon. The Achilles tendon is a strong band of tissue that connects the calf muscles to the heel bone. Often, a painful spur is present on the back of the heel. of the heel bone. It typically occurs where the plantar fascia, a thick band of tissue that connects the heel bone to the toes, attaches to the heel.
of the heel bone. It typically occurs where the plantar fascia, a thick band of tissue that connects the heel bone to the toes, attaches to the heel. your foot connects to your leg. It can range from mild to severe and may be caused by various factors such as injury, inflammation, or medical conditions. The pain can make it difficult to walk, stand, or put weight on the affected ankle.
your foot connects to your leg. It can range from mild to severe and may be caused by various factors such as injury, inflammation, or medical conditions. The pain can make it difficult to walk, stand, or put weight on the affected ankle. feet, it can cause significant discomfort and affect your ability to walk or stand properly. It may result from accidents, falls, or overuse injuries. Common symptoms of a foot fracture include pain, swelling, bruising, and difficulty bearing weight on the affected foot. Treatment usually involves immobilizing the foot with a cast, brace, or splint to allow the bone to heal. In some cases, surgery may be required. It’s important to seek medical attention for proper diagnosis and treatment of a foot fracture to ensure proper healing and prevent long-term complications. If you think that you may have this
feet, it can cause significant discomfort and affect your ability to walk or stand properly. It may result from accidents, falls, or overuse injuries. Common symptoms of a foot fracture include pain, swelling, bruising, and difficulty bearing weight on the affected foot. Treatment usually involves immobilizing the foot with a cast, brace, or splint to allow the bone to heal. In some cases, surgery may be required. It’s important to seek medical attention for proper diagnosis and treatment of a foot fracture to ensure proper healing and prevent long-term complications. If you think that you may have this  which are strong bands of tissue that connect bones together, get stretched or torn. This can happen due to sudden twisting or rolling of the foot, causing pain, swelling, and difficulty in walking or putting weight on the affected foot. The foot may feel unstable, and there may be a sensation of the foot giving way.
which are strong bands of tissue that connect bones together, get stretched or torn. This can happen due to sudden twisting or rolling of the foot, causing pain, swelling, and difficulty in walking or putting weight on the affected foot. The foot may feel unstable, and there may be a sensation of the foot giving way. is a thick cord-like structure that connects muscles to bones. It commonly occurs due to overuse or repetitive movements, such as in sports or repetitive job tasks. Tendonitis can cause pain, tenderness, and swelling in the affected area, making it difficult to move the associated joint. Rest, ice, and anti-inflammatory medications are often recommended for initial treatment. Modifying activities, stretching, and physical therapy exercises can help alleviate symptoms and promote healing. In severe cases, a healthcare professional may suggest additional interventions such as corticosteroid injections or, rarely, surgery. It’s important to rest and seek medical advice for proper diagnosis and treatment of tendonitis to prevent further complications.
is a thick cord-like structure that connects muscles to bones. It commonly occurs due to overuse or repetitive movements, such as in sports or repetitive job tasks. Tendonitis can cause pain, tenderness, and swelling in the affected area, making it difficult to move the associated joint. Rest, ice, and anti-inflammatory medications are often recommended for initial treatment. Modifying activities, stretching, and physical therapy exercises can help alleviate symptoms and promote healing. In severe cases, a healthcare professional may suggest additional interventions such as corticosteroid injections or, rarely, surgery. It’s important to rest and seek medical advice for proper diagnosis and treatment of tendonitis to prevent further complications.
 tapes or bandages to support and stabilize the feet or ankles. It is commonly used to provide temporary relief and prevent further injury in conditions such as sprains, strains, or ligament instability. The tape is applied in specific patterns to restrict excessive movement, reduce pain, and improve joint stability. Strapping can also help to alleviate pressure on certain areas of the foot or provide support to weakened or injured structures. It is usually performed by a podiatrist or trained healthcare professional who has knowledge of proper taping techniques. The strapping is typically temporary and may need to be reapplied periodically depending on the individual’s condition and healing progress. In addition to strapping, podiatrists may offer
tapes or bandages to support and stabilize the feet or ankles. It is commonly used to provide temporary relief and prevent further injury in conditions such as sprains, strains, or ligament instability. The tape is applied in specific patterns to restrict excessive movement, reduce pain, and improve joint stability. Strapping can also help to alleviate pressure on certain areas of the foot or provide support to weakened or injured structures. It is usually performed by a podiatrist or trained healthcare professional who has knowledge of proper taping techniques. The strapping is typically temporary and may need to be reapplied periodically depending on the individual’s condition and healing progress. In addition to strapping, podiatrists may offer  are designed to support and improve the alignment of the feet. They are commonly prescribed by podiatrists to address various foot conditions, such as flat feet, high arches, plantar fasciitis, and other abnormalities. Orthotics can help distribute pressure evenly, provide stability, and correct foot posture while walking or standing. They are typically made from materials like foam, gel, or rigid plastic, and can be inserted into regular footwear. Orthotics can help alleviate foot pain, improve function, and prevent further foot-related problems. They are customized based on an individual’s specific foot shape and condition, and are typically fitted and prescribed by a podiatrist or foot specialist. In addition to orthotics, podiatrists may offer
are designed to support and improve the alignment of the feet. They are commonly prescribed by podiatrists to address various foot conditions, such as flat feet, high arches, plantar fasciitis, and other abnormalities. Orthotics can help distribute pressure evenly, provide stability, and correct foot posture while walking or standing. They are typically made from materials like foam, gel, or rigid plastic, and can be inserted into regular footwear. Orthotics can help alleviate foot pain, improve function, and prevent further foot-related problems. They are customized based on an individual’s specific foot shape and condition, and are typically fitted and prescribed by a podiatrist or foot specialist. In addition to orthotics, podiatrists may offer  inserts intended for individuals with diabetes. These products are created to provide comfort, support, and reduce the risk of foot complications associated with diabetes. Diabetic shoes have features like extra depth, wide toe boxes, and soft, seamless interiors to accommodate any foot deformities, swelling, or neuropathy (nerve damage). They are typically made from breathable materials to prevent excessive moisture and promote circulation. Diabetic insoles, on the other hand, are inserts that fit inside regular shoes and provide additional cushioning, shock absorption, and pressure redistribution to protect the feet. Both diabetic shoes and insoles aim to reduce the risk of ulcers, sores, and other foot injuries that can lead to serious complications. It is recommended for individuals with diabetes to consult with a podiatrist or healthcare professional to assess their specific needs and determine if diabetic shoes or insoles, along with
inserts intended for individuals with diabetes. These products are created to provide comfort, support, and reduce the risk of foot complications associated with diabetes. Diabetic shoes have features like extra depth, wide toe boxes, and soft, seamless interiors to accommodate any foot deformities, swelling, or neuropathy (nerve damage). They are typically made from breathable materials to prevent excessive moisture and promote circulation. Diabetic insoles, on the other hand, are inserts that fit inside regular shoes and provide additional cushioning, shock absorption, and pressure redistribution to protect the feet. Both diabetic shoes and insoles aim to reduce the risk of ulcers, sores, and other foot injuries that can lead to serious complications. It is recommended for individuals with diabetes to consult with a podiatrist or healthcare professional to assess their specific needs and determine if diabetic shoes or insoles, along with  skin of the feet, particularly between the toes. It is characterized by symptoms such as itching, burning, redness, and peeling skin. The infection is caused by fungi that thrive in warm and moist environments, such as sweaty shoes or public showers. Athlete’s foot is a common
skin of the feet, particularly between the toes. It is characterized by symptoms such as itching, burning, redness, and peeling skin. The infection is caused by fungi that thrive in warm and moist environments, such as sweaty shoes or public showers. Athlete’s foot is a common  response to repeated pressure or friction.
response to repeated pressure or friction. tissue, most commonly occurring in the foot, between the metatarsal bones. It is often referred to as Morton’s neuroma. The thickening typically happens around the nerve that runs between the third and fourth toes.
tissue, most commonly occurring in the foot, between the metatarsal bones. It is often referred to as Morton’s neuroma. The thickening typically happens around the nerve that runs between the third and fourth toes. occurs in a bone. It is often caused by repetitive stress or overuse of the bone, commonly seen in athletes or individuals who engage in activities with high impact or repetitive movements.
occurs in a bone. It is often caused by repetitive stress or overuse of the bone, commonly seen in athletes or individuals who engage in activities with high impact or repetitive movements. are caused by a viral infection. They are typically non-cancerous and can occur on various parts of the body, such as the hands, feet, and face.
are caused by a viral infection. They are typically non-cancerous and can occur on various parts of the body, such as the hands, feet, and face. the feet. These wounds can result from various causes, such as diabetes, poor circulation, pressure, or injury. Podiatrists specialize in assessing and treating these wounds to promote healing and prevent complications. Wound care involves cleaning the wound, removing any dead tissue, and applying appropriate dressings or bandages to protect the area and promote healing. Podiatrists may also recommend offloading techniques to reduce pressure on the wound, such as padding or specialized footwear. In the case of diabetic foot ulcers, additional measures like infection management and blood sugar control may be necessary. Regular monitoring and follow-up visits are essential to ensure proper healing and prevent infection or further complications.
the feet. These wounds can result from various causes, such as diabetes, poor circulation, pressure, or injury. Podiatrists specialize in assessing and treating these wounds to promote healing and prevent complications. Wound care involves cleaning the wound, removing any dead tissue, and applying appropriate dressings or bandages to protect the area and promote healing. Podiatrists may also recommend offloading techniques to reduce pressure on the wound, such as padding or specialized footwear. In the case of diabetic foot ulcers, additional measures like infection management and blood sugar control may be necessary. Regular monitoring and follow-up visits are essential to ensure proper healing and prevent infection or further complications.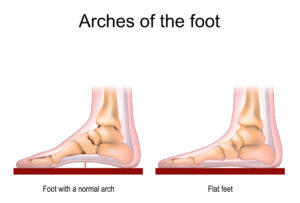 the arches on the inside of the feet are flattened, causing the entire sole of the foot to touch the ground when standing.
the arches on the inside of the feet are flattened, causing the entire sole of the foot to touch the ground when standing. pain in the heel or bottom of the foot. It occurs when the plantar fascia, a thick band of tissue that connects the heel bone to the toes, becomes inflamed or irritated.
pain in the heel or bottom of the foot. It occurs when the plantar fascia, a thick band of tissue that connects the heel bone to the toes, becomes inflamed or irritated. Bunions are a common
Bunions are a common 
 bend or curl downward instead of pointing straight. The affected toes resemble a hammer or a claw.
bend or curl downward instead of pointing straight. The affected toes resemble a hammer or a claw. surrounding skin instead of growing straight. This can lead to pain, redness, swelling, and possible infection.
surrounding skin instead of growing straight. This can lead to pain, redness, swelling, and possible infection. the base of the big toe becomes stiff, painful, and less flexible. It is a common
the base of the big toe becomes stiff, painful, and less flexible. It is a common 


